

In such situations, arterial measurement may be more appropriate.Īcute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, et al. This is particularly relevant for traumatic brain injury, where high carbon dioxide can lead to raised intracranial pressure, whilst low carbon dioxide can lead to cerebral ischaemia. Given that in unstable patients, the gradient is more significant than previously thought and that there is a lack of a predictable relationship, the ETCO 2 is not a suitable stand-in for the PaCO 2 where pH or PaCO 2 requires precise control. Moreover, a correlation has only been moderate, meaning there is variation between the levels, making it difficult to predict the difference in the gradient. This has been observed to result in patients with high or low CO 2 being misclassified as having normal CO 2.
More recent studies have demonstrated the gradient in unstable patients exceeds the expected difference of 0.5 kPa (3.8 mmHg). However, in the presence of ventilation-perfusion mismatch, acid-base disturbance, and haemodynamic instability, this difference may increase.
These guidelines are based upon evidence which has been extrapolated from healthy individuals, often in the controlled setting of an operating theatre.

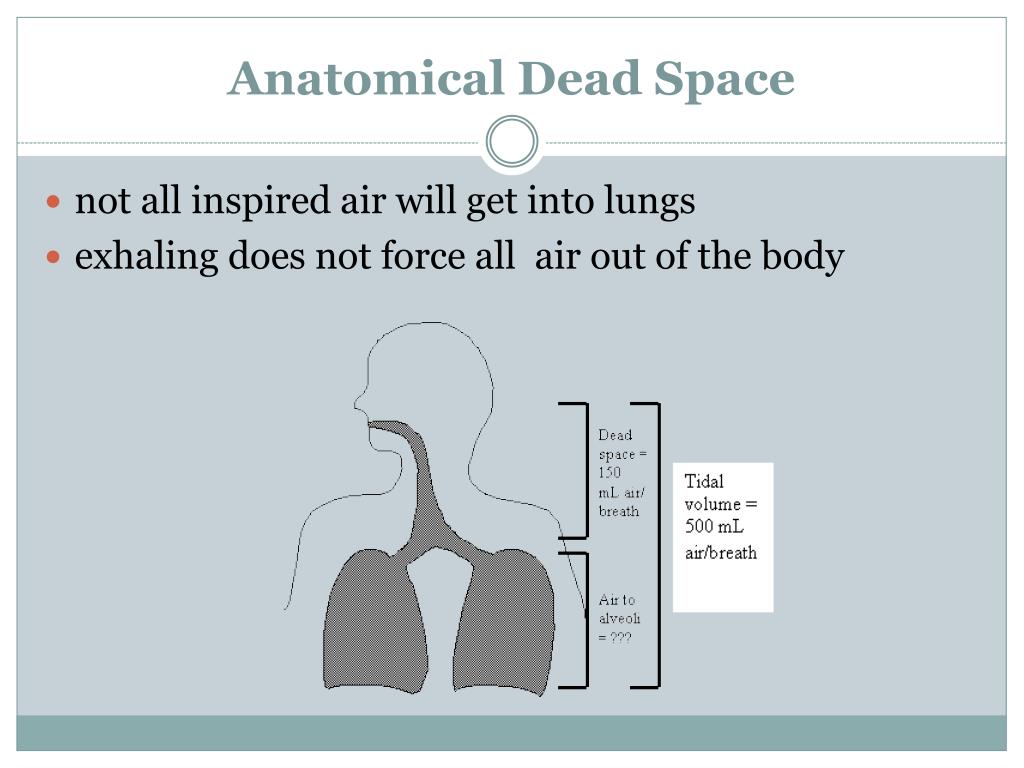
This model predicts that gas exchange with volumes smaller than dead space should vary approximately as the product of f and VT2.Can the PaCO2- ETCO2 gradient be predicted?Ĭurrent guidance recommends an ETCO2 of 4.0–4.5 kPa (30.0–33.8 mmHg) as a stand-in for a low-normal PaCO 2 with an expected difference of 0.5 kPa (3.8 mmHg). At tidal volumes less than 7 ml/kg, the data deviated substantially from the conventional alveolar ventilation equation but fit well a model derived previously for HFV. The frequency required to maintain constant alveolar ventilation increased slowly as tidal volume was decreased from 15 to 7 ml/kg but rose sharply with attendant rapid increases in minute ventilation as tidal volumes were decreased to less than 7 ml/kg. We found that VD was relatively constant at tidal volumes associated with normal ventilation (7-15 ml/kg) but fell sharply as VT was reduced further to tidal volumes associated with HFV (less than 7 ml/kg). We quantified changes in VD in three dogs at constant alveolar ventilation using the Bohr equation as VT was varied from 3 to 15 ml/kg and frequency (f) from 0.2 to 8 Hz, ranges that include normal as well as HFV. Tidal volumes used in high-frequency ventilation (HFV) may be smaller than anatomic dead space, but since gas exchange does take place, physiological dead space (VD) must be smaller than tidal volume (VT).


 0 kommentar(er)
0 kommentar(er)
